Tissues are composed of cells with different functions and shapes. Variation of inter-cell interaction, their position, their structure and their organization may account either for ordinary, physiological cell transformation, or for the possible presence of pathologic alterations.
An accurate microscopic tissue analysis may show histological and functional variations in tissues or organs and thus disclose the presence and the evolution of such processes.
In order to prepare good-quality histological specimens, the selected tissue must be prepared carefully according to the following stages:
1. Fixation
2. Embedding
3. Sectioning
4. Staining
5. Microscopy visualization
1. Fixation. After the sample has been collected through postmortem collection or in vivo biopsy, the first step is fixation. This is a very delicate procedure. Proper and accurate analysis of the tissue depend on preservation of cell organization and tissue components.
The aim of fixation is to avoid the disorganizing processes of cells and tissues. To achieve this purpose, fixation immediately kills the cells through chemical or physical processes, which inactivate the functions of enzymes and lytic bacteria, thus avoiding tissue degradation and keeping cellular organization intact.
There are multiple types of fixatives: for example, they can either be single components (such as formalin, picric acid and osmium tetroxide) or a solution of various fixatives (i.e. Bouin, Zenker, Susa). In the second case, the combination of more fixatives can take advantage of the different component features (such as penetration speed, decalcification, dye affinity) and may get a better fixative result. These combinations are called coagulant when they act by coagulating the proteins that are found in tissues (i.e. ethanol, picric acid, mercury chloride). Conversely, they are known as non-coagulant if they give rise to a jellification process of the various tissue components (formalin, osmium tetroxide).
Generally, the most commonly used chemical fixatives are 2.5% paraformaldehyde and Buoin, Zenker and Carnoy combinations. Chemical fixation is frequently combined with physical fixation; therefore, fixation is performed at 4°C in the refrigerator or at -20°C in the freezer.
In case results are needed urgently, for example in surgery, or in case cell proteins must not be denatured, cryofixation may be performed at -80°C with methyl butane or liquid nitrogen, including a special resin, the OCT. In this way, the sample can be stored in the freezer at -80°C and be followed by cryostat sectioning.
2. Embedding. The aim of this process is to store the anatomical samples in a solid medium, as inert as possible, in order to preserve them, so that they can be sectioned in different thicknesses. Depending on the investigation methods used afterwards, there are multiple embedding media that can be chosen. A very important benchmark in the choice of the embedding medium is the thickness of the tissue sections that are to be achieved. For example, semi thin sections (1-1.5 µm) are to be embedded in resins, such as glycol methacrylate (GMA) or methyl methacrylate (MMA). In case we need to achieve thicker sections (3-25 µm), it is necessary to use different combinations of paraffins. The melting point of such paraffins is approximately between 50°-52°C and 60°-62°C and their choice depends on various factors, such as environmental conditions, the tissue to be examined, its size and hardness. In general, the harder and larger the sample, the harder the combination must be. Finally, if the investigation of the sample involves some immunofluorescence labelling process, the best solution is the OCT, a plastic resin which solidifies at low temperatures.
3. Sectioning. The blocks obtained must be cut cleanly in sections of the appropriate thickness to be stained and analyzed with a microscope. The embedding method and the thickness to be achieved affect the choice of the sectioning tool. For example, if we want to produce semi-thin sections, we should opt for an ultramicrotome, a special microtome equipped with specific steel or diamond blades. For sections between 3 µm and 25 µm we can use a microtome, which allows the embedding blocks to slide over a blade. Rotary microtomes are to be used in the sectioning process if samples size is relatively small (4-12 µm), whereas sliding microtome are used for larger and thicker samples. In case OCT has been used in the embedding process, a cryostat represents the best solution: it is a microtome stored in a refrigerated container, at a temperature between -20°C and -40°C, which makes it possible to obtain sections between 5-20 µm.
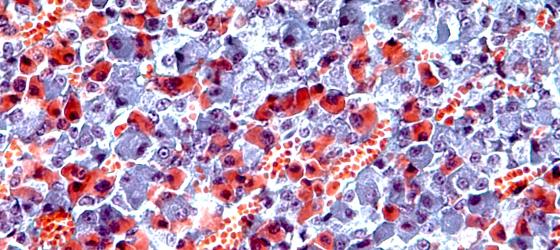
4. Staining. This is the process through which samples are placed on the slides and led to react with different compounds that bind and stain tissues components. Once they are stained, it is possible to analyze their morphology. Over time, staining categories with different features (different colors and/or reaction affinity) have been discovered. Such categories, even when combined, allow a better morphological analysis. In order to optimize the various methods, different staining techniques have been developed:
- Histological stainings, in which one or more dyes allow the morphological analysis of tissues;
- Histochemical stainings, in which chemical compounds react with specific components of the tissue and thus provide information about specific chemical substances in the biological tissue. The chemical reaction produced will result in a dyed precipitate directly on the section;
- Immunohistochemical stainings, in which antibodies label some specific components in the tissues. This category is highly selective because it relies on the highly specific reaction between antibody and antigen (possibly present in the tissue);
- Immunofluorescence stainings (variant of the immunohistochemical staining), in which secondary antibodies are bound to fluorochromes which¸ after being exposed to an excitation source, emit light with specific wavelengths that can be detected using a confocal or fluorescence microscope.
5. Microscope visualization. In order to make a diagnosis and to provide the corresponding photographic evidence, we need not only a solid theoretical knowledge of tissues, but also a proper expertise on our investigation instrument: the light microscope.
Light microscopes are equipped with:
- Base,
- Ocular lenses,
- Objective lenses,
- Macrometric and micrometric screws.
The proper use of these components allows us to exploit the full potential of this instrument.
When using the microscope, we need to follow the steps mentioned below:
- adjust the ocular lenses to your interpupillary distance by enlarging or approaching them;
- adjust light through the potentiometer. Its intensity should never be too high;
- place the slide on the stage and focus with the smaller objective. In general, the nosepiece includes five objectives: 4x, 10x, 20x, 40x and 100x. It is important to start the visualization phase with the lower magnification level in order to get a general view of the specimen, its staining and its state of preservation.
Once we have carried out the adjustments, the specimen is ready to be analyzed, by keeping in mind these suggestions:
- start the visualization on the free margin of the specimen, no matter whether it is connective, capsular or covering epithelium, so that a sharp and neat view can be obtained (with regard to solid organs, the free margin is represented by their outermost part, which is generally covered by a connective capsule. In the case of hollow organs, the free margin is the inner surface of the cavity, covered by epithelium). If the size is large, as for liver, spleen and lungs, the free margin cannot be appreciated;
- after the first examination with lower levels of magnification we can proceed to a further analysis through the other objectives (i.e. 20x or 40x), so that we can provide a more thorough diagnosis;
- in order to achieve an adequately magnified visualization of blood smears, lung sputa or semen, at least the 40x must be used;
- to achieve the ultimate magnification, it is necessary to multiply the ocular resolution (always 10x) by the resolution of the various objectives. In this way, if we observe with objective 4, we will see the specimen enlarged 40 times (magnification 10 of the ocular, multiplied by 4, objective magnification = magnification 40x). If we observe with objective 10, we will see the specimen enlarged 100 times, and so on. For convenience purposes, we will replace the word magnification with X, so that we will refer to specimen observed at X40, X100, X200, etc.