The cells composing this tissue derive from the epithelial lining. They can either be found in the mucosal and submucosal tunica of hollow organs or they can compose the whole organ themselves.
If the gland maintains any connection with the free surface through excretory ducts and secretes its compound on the epithelium, then it is called exocrine gland. Whereas, if there is no duct and its compound is discharged into the blood system, the gland is known as endocrine gland (the substance produced by such glands is generally defined as hormone).
Although the majority of glands has an epithelial origin, there are some exceptions: for example, there are hormone-secreting cells, deriving from connective tissue (interstitial cells of gonads, theca folliculi cells, or adipocytes). Glands can also have a nervous origin (known as neuroendocrine, e.g. the magnocellular and parvocellular systems of the hypothalamus), or muscular origin (for example, the cardiac myocytes producing the atrial natriuretic factor –ANF).
Glandular secretion can be either rhythmic or non-rhythmic.
With rhythmic secretion, the substance is expelled outside the cell as it is produced, for example endocrine glands secreting steroid hormones.
In case of non-rhythmic secretion, on the other hand, the substance is stored in the form of exocytosis granules inside the cell and subsequently expelled after receiving a hormonal, nervous or chemical impulse.
Exocrine glands
Exocrine glands are composed of a secreting part, known as adenomere, and an excretory duct, whose function is to expel the substance outside the gland.
Exocrine glands can be classified depending on various criteria:
Depending on the number of cells constituting the adenomere.
In this case, two types can be distinguished: unicellular and multicellular glands.
Depending on the number and branchings of the excretory ducts
In case an adenomere presents only one excretory duct, the gland is a simple gland. Whereas, if several adenomeres present only one excretory duct, the gland is a branched gland. Finally, if several draining excretory ducts firstly converge in each other and then towards a common excretory duct, this is a compound gland.
Depending on the shape of the adenomere
In case the adenomere has an elongated shape and presents a quite prominent lumen, glands are called tubular glands; among them, a particular example is represented by tubule-glomerular glands, which uniquely correspond to sweat glands. If the shape of the adenomere is round, small and, therefore, hardly visible, the gland is acinar. In case the adenomere is round, large and clearly visible, the gland is called alveolar. In branched glands, there might be a combination of tubular adenomeres and either acinar (tubuloacinar glands) or alveolar adenomeres (tubuloalveolar glands).
Depending on the mechanism of secretion
- Merocrine (or eccrine) secretion: the secretory product is released through the cytoplasmic membrane (exocytocis). In this way, the cell remains intact, e.g. parotid, exocrine pancreas and salivary glands.
- Apocrine secretion: part of the cytoplasm, surrounded by the cytoplasmic membrane, is lost during the secretory phase and becomes part of the secreted substance; here are some examples: mammary glands (limited to lipid secretion), sweat glands with a wide lumen.
- Holocrine secretion: the substance is expelled in the excretory duct due to the disintegration of the cell itself, e.g. sebaceous cells.
Depending on the type of secretion (only in merocrine glands)
Serous glands (in case the secretory substance is mainly composed of proteins and water), mucous glands (in which the secretory substance is mainly composed of glycoproteins and water) and seromucous glands (mixed).
Depending on their topographic collocation
There may be either intraepithelial or extraepithelial glands. The second type is divided into parietal and extraparietal glands.
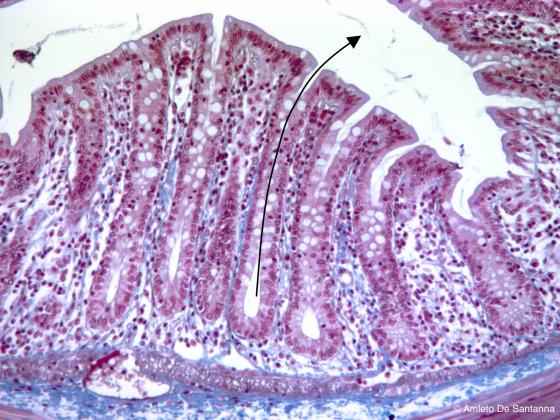
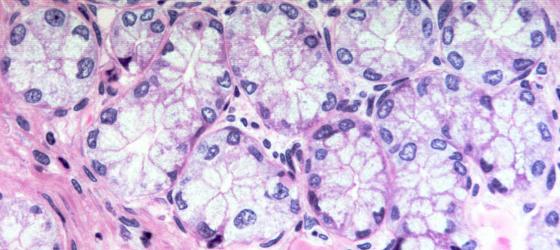
Figure E105. Rat colon. Intestinal glands (crypts of Lieberkühn). These are exocrine simple tubular glands that open onto the luminal surface (the arrow shows the glandular lumen and the direction of the secrete). In this manner, the secretion product is directly poured into the lumen. Mallory-Azan X100
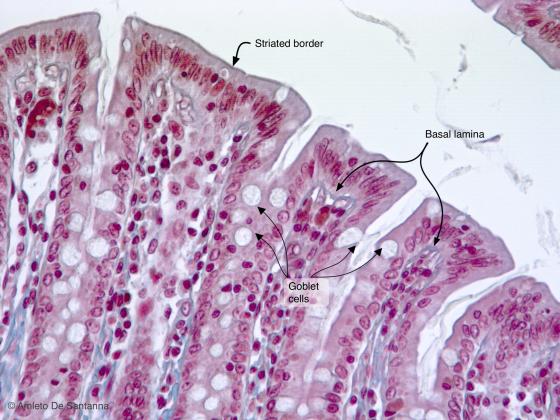
Figure E106. Rat colon. Intestinal glands (or crypts of Lieberkühn) at high magnification. These glands are simple tubular glands that open onto the surface of the intestinal lumen. The lining epithelium is simple columnar with brush border and presents many interposed goblet cells . Mallory-Azan X200
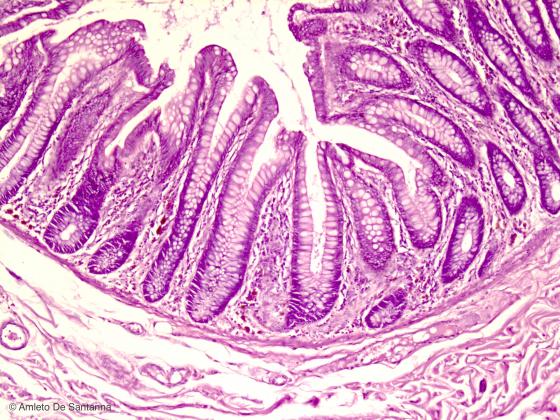
Figure E107. Human small intestine. You can see the villi lined by simple columnar epithelium where we find many goblet cells. Goblet cells are unicellular exocrine glands that secrete mucus. H&E X40
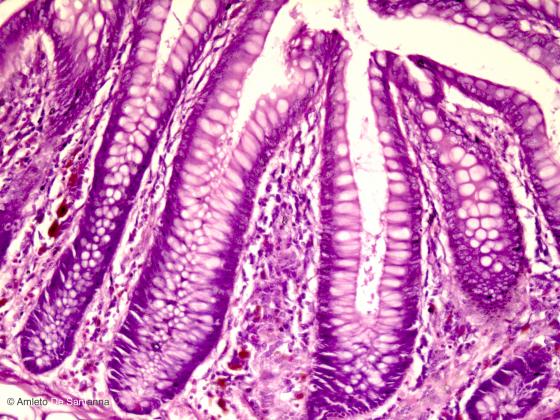
Figure E108. Human small intestine at higher magnification. H&E X100
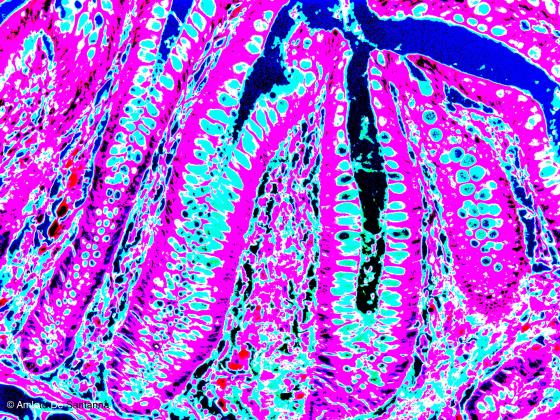
Figure E109. Human small intestine at higher magnification. The micrograph has been digitally modified to make the goblet cell mucus easily visible (light blue). X100
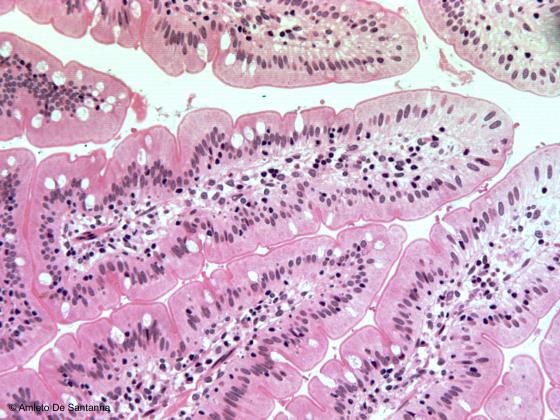
Figure E110. Human small intestine. Simple columnar epithelium composed of enterocytes with microvilli in the apical domain and goblet cells. Goblet cells are unicellular, intraepithelial, exocrine glands that excrete mucus in order to lubricate and protect the luminal surface of the hollow organ. Because of the high content of mucus, that is hydrophobic, the goblet cells are colorless or only slightly stained when conventional staining methods are used. H&E X100
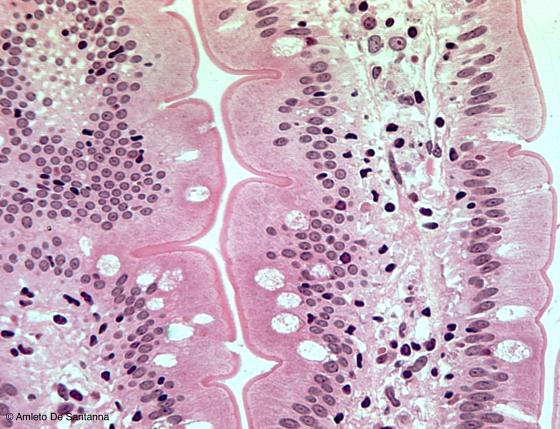
Figure E111. Human small intestine. Micrograph at high magnification where you can see the enterocytes interspersed with goblet cells that have an intracellular voluminous amount of colorless mucus. H&E X200
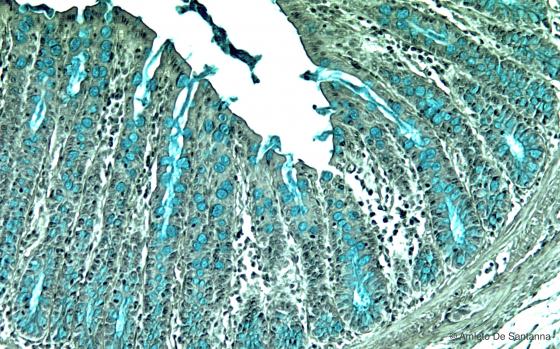
Figure E112. Rat colon. Simple columnar epithelium consisting of enterocytes and goblet cells stained with alcian blue.This is a selective method for mucins that are stained bright blue. Alcian blu-hematoxylin X100
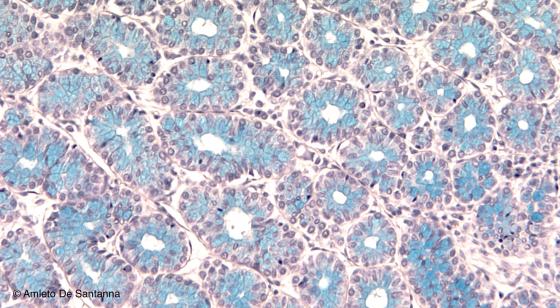
Figure E113. Rat colon. Transversal section where you can see many goblet cells. Alcian blue-hematoxylin X100
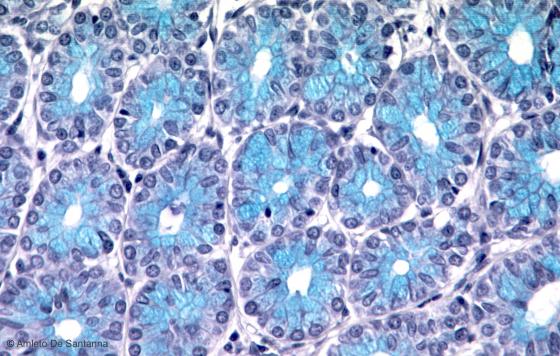
Figure E114. Mouse colon. Transverse section of the intestinal glands (crypts of Lieberkühn). You can see the excreting tubules of the glands. This staining method highlights the mucus of the goblet cells (bright blue). Alcian blue-hematoxylin X200
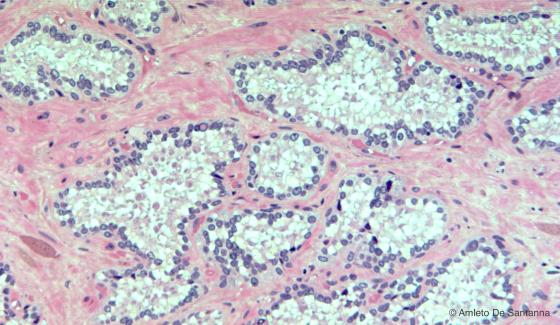
Figure E115. Human seminal vesicles. Seminal vesicles are the simplest form of exocrine multicellular gland, where the whole lining epithelium is made of excreting cells. In addition, the gastric mucosa and the endometrium of the uterus have this kind of organization. H&E X100
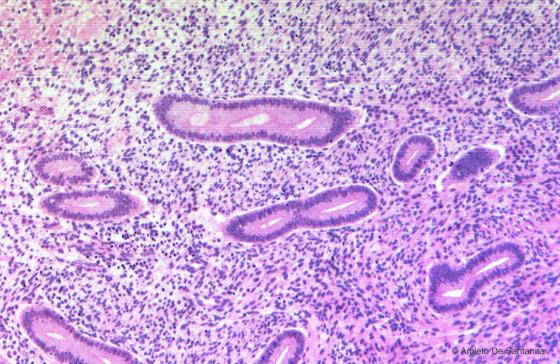
Figure E116. Endometrium of human uterus in the proliferative phase. Another example where the whole lining epithelium is made of excreting cells. H&E X63

Figure E117. Human stomach. Pyloric region. H&E X100
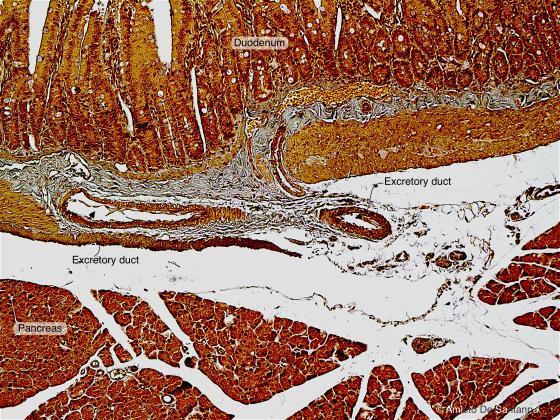
Figure E118. Rat duodenum. Large excretory duct lined by simple columnar epithelium. Ignesti X12.5
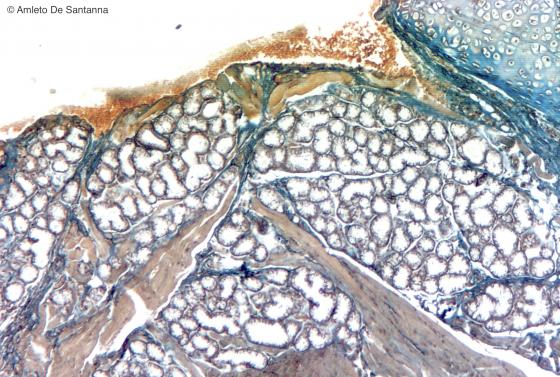
Figure E119. Human sublingual gland. Compound tubular exocrine glands that produce a mucous secretion. Ignesti X63
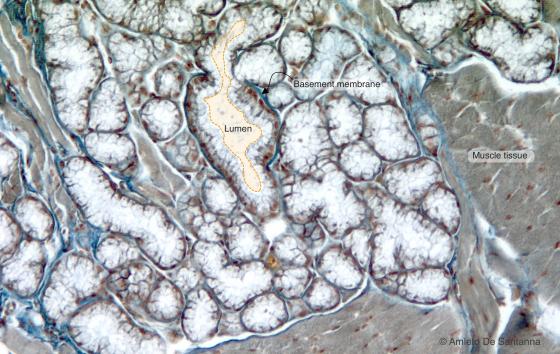
Figure E120. Human sublingual gland at higher magnification. You can see the stretched secretory portion with an easily visible lumen. The cells have an elongated, flattened nucleus at the base and a colorless cytoplasm. Ignesti X100
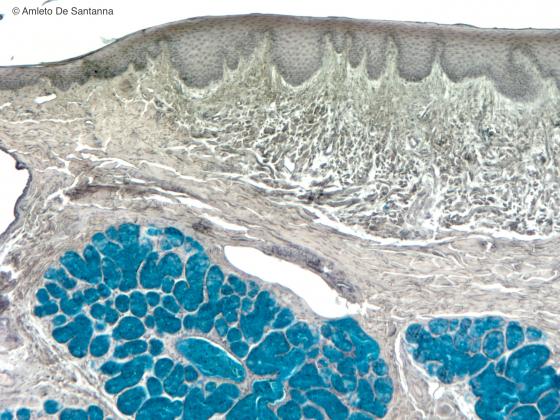
Figure E121. Human soft palate. Selective staining method for mucus that is stained bright blue. Alcian blue-hematoxylin X63
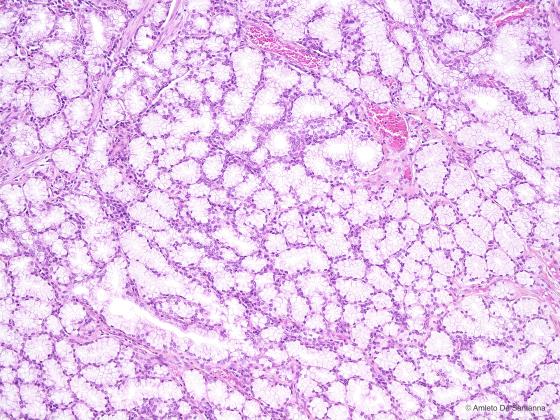
Figure E122. Human duodenum. Brunner’s glands. These glands are exocrine glands located in the submucosa of the duodenum that secrete an alkaline mucus. H&E X100
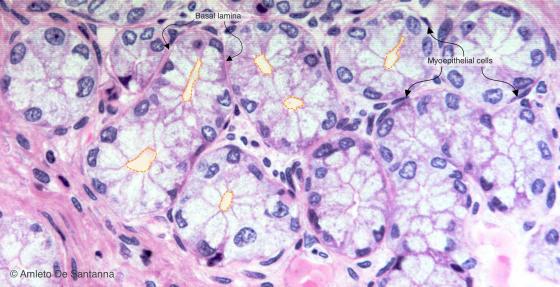
Figure E123A. Human duodenum. Brunner’s glands at higher magnification. The easily visible (shaded orange) gland lumen is typical of the tubular glands and make them distinguishable from acinar glands also in transverse section. The cytoplasm of the cells of the secreting units is very pale. A flattened nucleus at the base of the cells is a feature that makes glands with a mucous secretion unmistakable. H&E X200
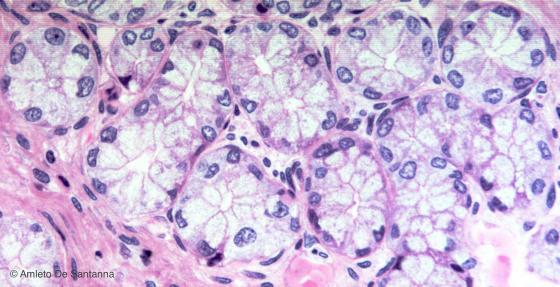
Figure E123B. Human duodenum. Brunner’s glands at higher magnification. H&E X200
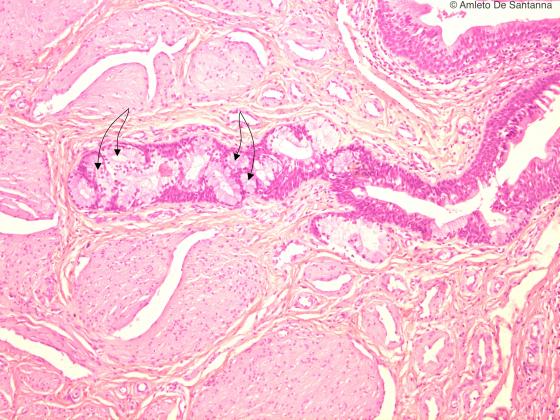
Figure E124. Human penile urethra. Urethral glands. These tubular glands excrete mucus (arrows). H&E X100
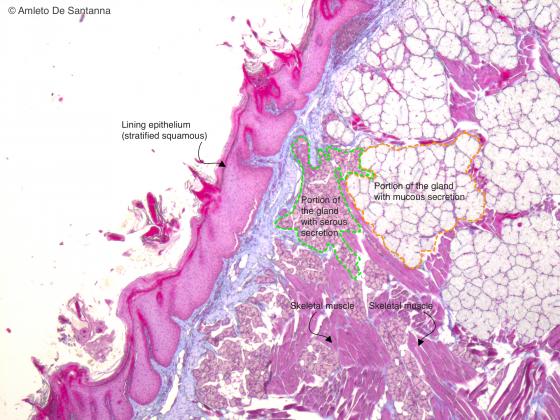
Figure E125A. Human fetal tongue. You can see different types of exocrine glands: tubular glands with a mucous secretion (paler) and acinar glands with a serous secretion (darker). Mallory-Azan X100
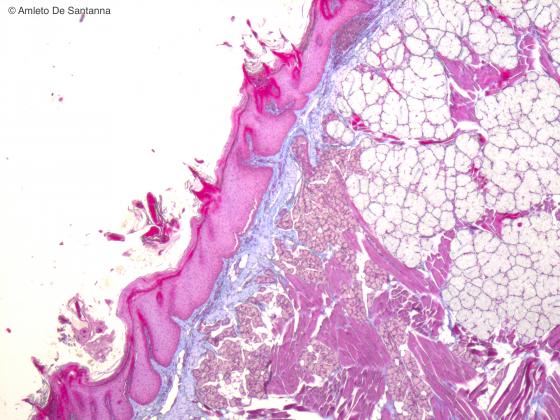
Figure E125B. Human fetal tongue. You can see different types of exocrine glands: tubular glands with a mucous secretion and acinar glands with a serous secretion. Mallory-Azan X100
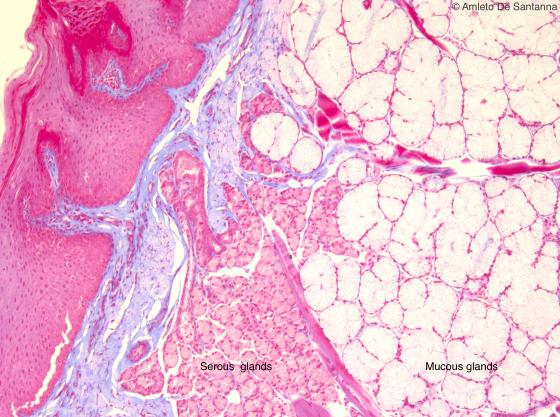
Figure E126. Human fetal tongue at higher magnification. You can see the different morphology of the two types of exocrine glands. You can distinguish the tubular glands with mucous secretion from acinar glands with serous secretion because the first have an elongated secretory unit, an evident lumen, a flattened nucleus located at the base of the cell and a pale cytoplasm, whereas the latter have a hardly visible lumen, a round nucleus located at the center of the cell and a strongly stained cytoplasm. Mallory-Azan X200
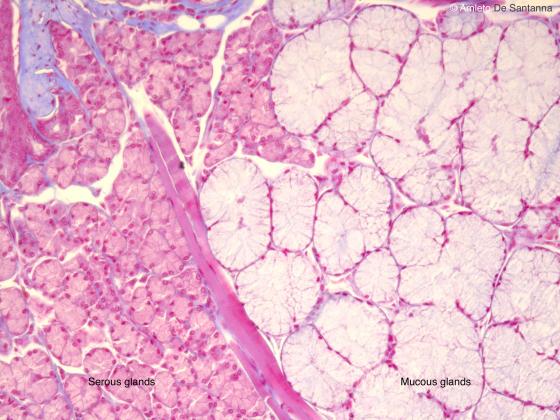
Figure E127. Human fetal tongue at higher magnification. Mallory-Azan X200
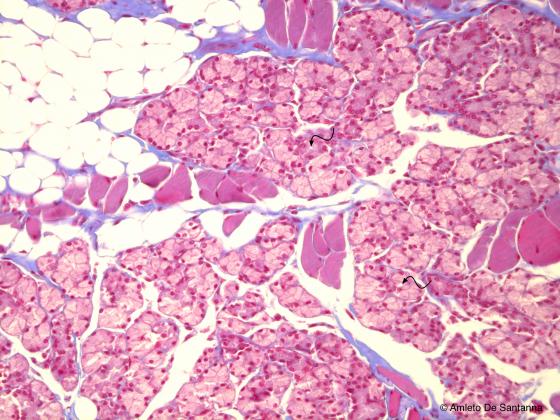
Figure E128. Human fetal tongue. Von Ebner’s gland. Compound acinar exocrine gland with serous secretion. Mallory-Azan X200
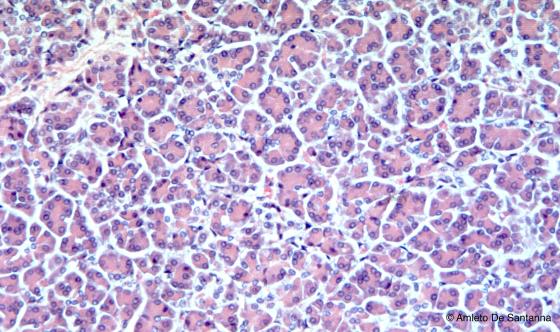
Figure E129. Human pancreas. Exocrine component of the pancreas. Compound acinar gland made of pancreatic acini with exclusively serous secretion H&E X100
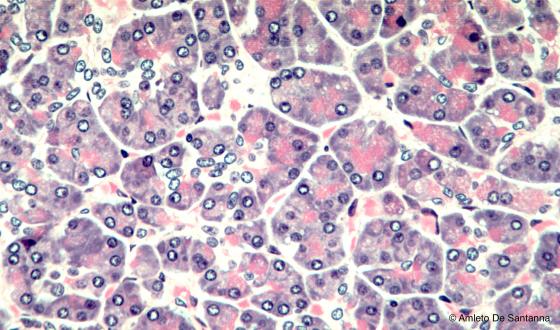
Figure E130. Human pancreas. High magnification of secretory units of a compound acinar exocrine gland with serous secretion. You can notice that the lumen of the acinus is hardly visible, and that the secreting cells have a round nucleus and a brightly stained cytoplasm. H&E X200
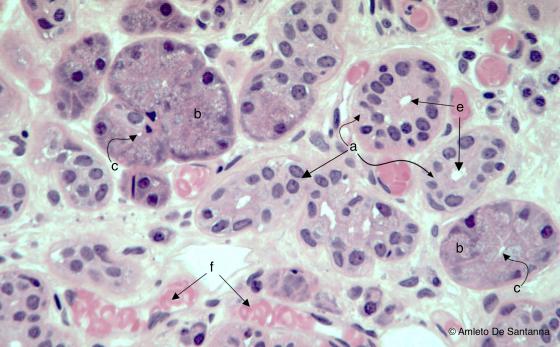
Figure E131. Human parotid gland. The parotid gland is a compound serous exocrine acinar gland. You can see the different morphology of: (a) the excretory ducts, which have an evident lumen lined by a cuboidal or columnar epithelium; (b) the secretory units, made of more deeply stained secreting cells with a cytoplasm in which the secretory granules are highly evident. The secretory units have small and hardly visible lumen (c), whereas the duct lumen is always larger and more visible (e). You can see blood capillaries (f). H&E X200

Figure E132. Compound acinar exocrine serous-secreting gland at high magnification. The characteristic shape of the secreting cells and the secretory granules are obvious. H&E X1000

Figure E133. Compound acinar exocrine serous-secreting gland at high magnification. Also in this micrograph, the characteristic morphology of the secreting cell is obvious. H&E X1000
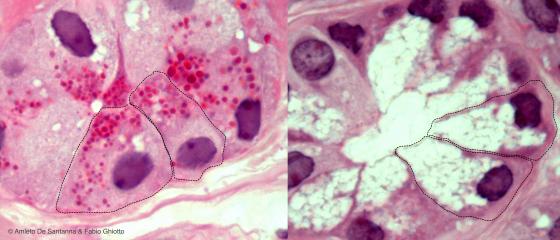
Figure E134. Assembling of two micrographs that compare serous-secreting cells (on the left) with mucus-secreting cells (on the right). The cells that compose the serous secretory portions of the gland are intensely stained because of the large amount of rough-surfaced endoplasmic reticulum and proteins. The cells of the mucus-secreting glands are generally poorly stained because the cytoplasm contains mucin droplets that are lost during the preparation of the sample, leaving empty spaces inside the cells. H&E
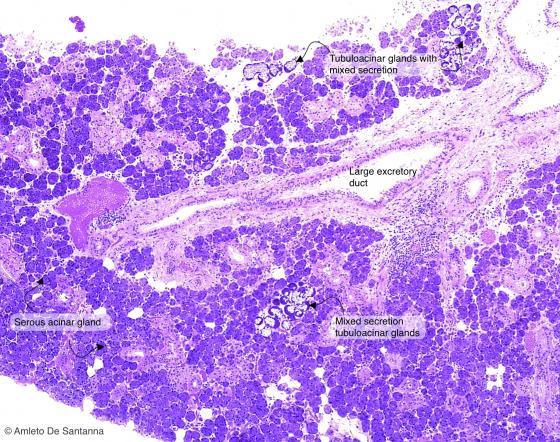
Figure E135. Human submandibular gland. Compound tubuloacinar gland with both serous-secreting and mucus-secreting cells. In routine preparations, the serous-secreting cells are squeezed out forming the serous demilunes (of Giannuzzi). H&E X40
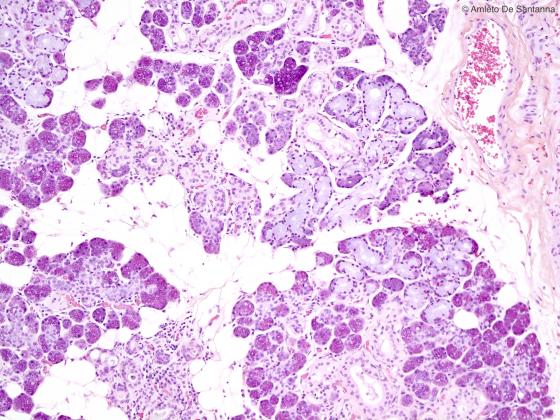
Figure E136. Human submandibular gland. Compound tubuloacinar gland with both serous-secreting and mucus-secreting cells. H&E X40

Figure E137. Human submandibular gland. Compound tubuloacinar gland with both serous-secreting and mucus-secreting cells. H&E X200
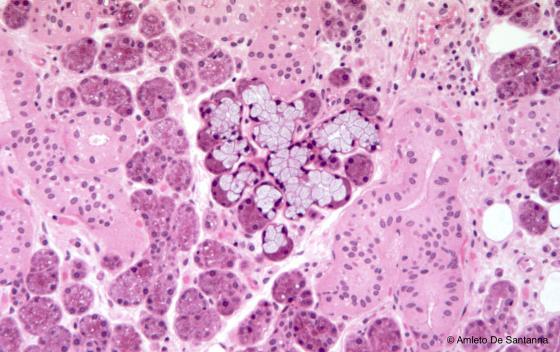
Figure E138. Human submandibular gland. Compound tubuloacinar gland with both serous-secreting and mucus-secreting cells. H&E X63
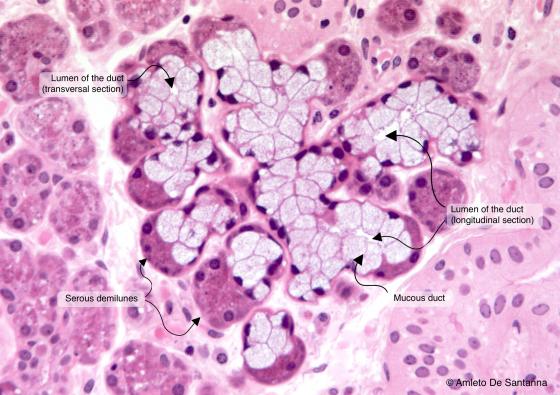
Figure E139A. Human submandibular gland at higher magnification. The tubular mucus-secreting units of the gland are elongated, pale and with an evident lumen. The acinar serous-secreting units of the gland are roundish with a hardly visible lumen and the cells have a centrally located nucleus and a deeply stained cytoplasm. In routine preparations, the acinar serous-secreting units are located on top of the tubular mucus-secreting units, like a hat: these formations are called demilunes. H&E X200
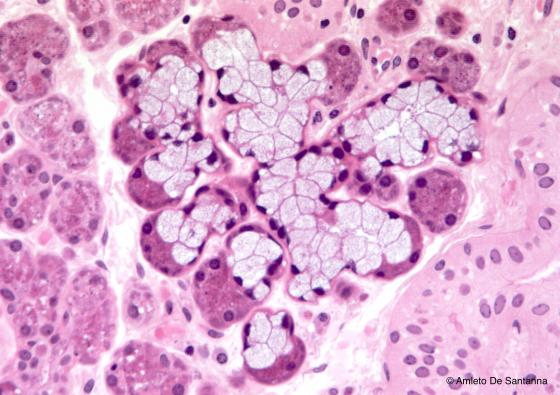
Figure E139B. Human submandibular gland at higher magnification. The tubular mucus-secreting units of the gland are elongated, pale and with an evident lumen. The acinar serous-secreting units of the gland are roundish with a hardly visible lumen and the cells have a centrally located nucleus and a deeply stained cytoplasm. In routine preparations, the acinar serous-secreting units are located on top of the tubular mucus-secreting units, like a hat: these formations are called demilunes. H&E X200
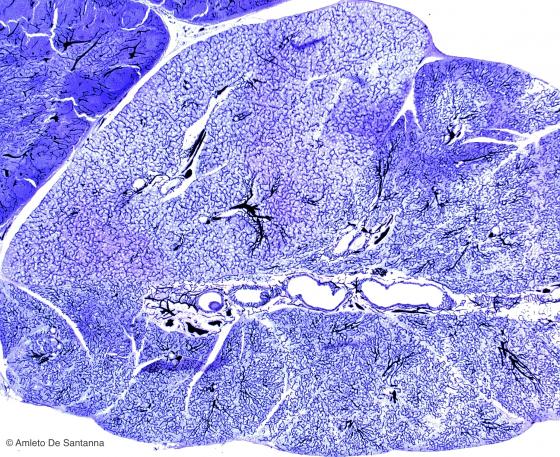
Figure E140. Mouse salivary gland. Vital staining with India ink that highlights the thick web of blood vessels that are present in the stroma of the gland. India ink X63
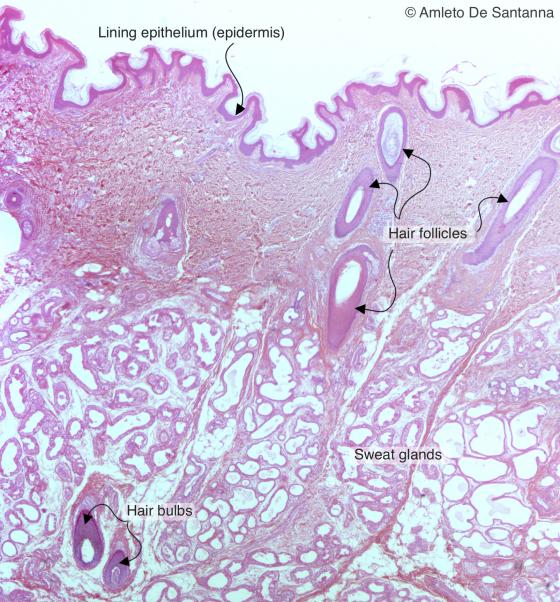
Figure E141. Human skin. Eccrine sweat glands (simple tubuloacinar glands) and apocrine sweat glands (branched tubular glands). H&E X12.5
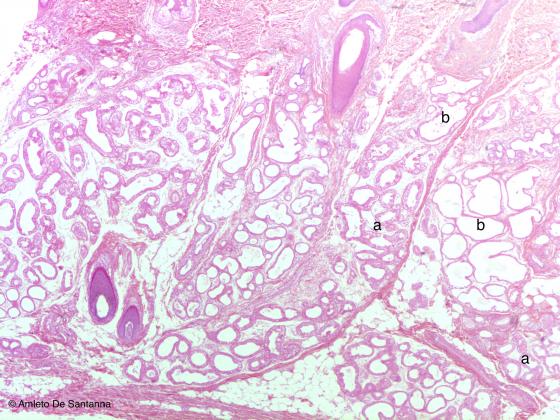
Figure E142. Human skin. Eccrine sweat glands, simple tubuloacinar glands (a), and apocrine sweat glands, branched tubular glands (b). H&E X25
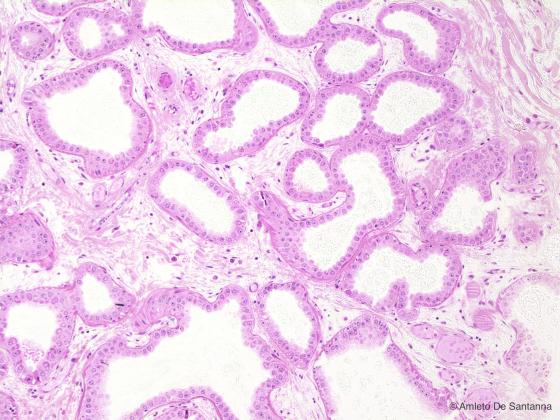
Figure E143. Human skin. Apocrine sweat gland. Branched tubuloacinar exocrine gland with a wide lumen. In the human kind, these glands are confined in few body regions: anus, pubes, areola of the nipple and the axillary region. H&E X40

Figure E144A. Human skin. Eccrine sweat gland. Simple tubuloacinar exocrine gland. The arrow depicts a possible course of the tubule. H&E X40
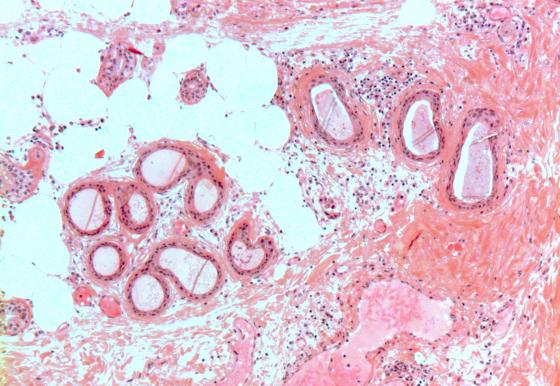
Figure E144B. Human skin. Eccrine sweat gland. Simple tubuloacinar exocrine gland. The arrow depicts a possible course of the tubule. H&E X40
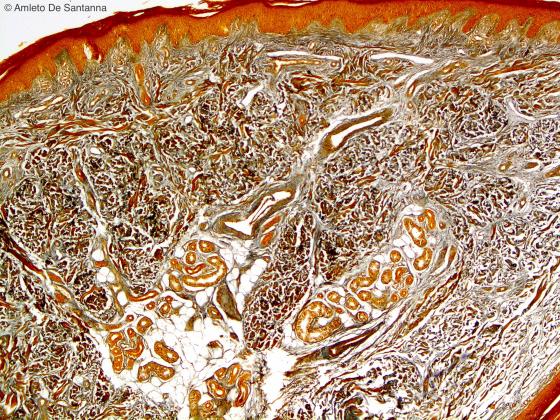
Figure E145. Human skin. You can see in the dermis several eccrine sweat glands. Ignesti X40
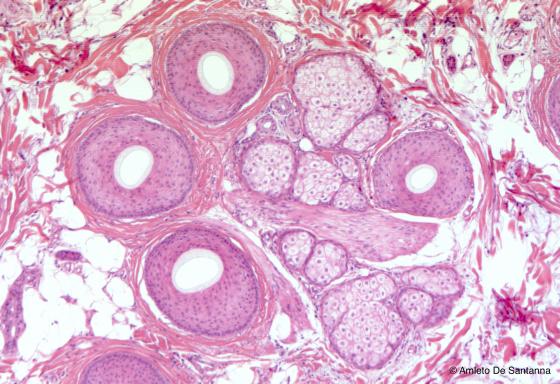
Figure E146. Human skin. Scalp in transverse section where you can see hair follicles surrounded by sebaceous glands. H&E X63
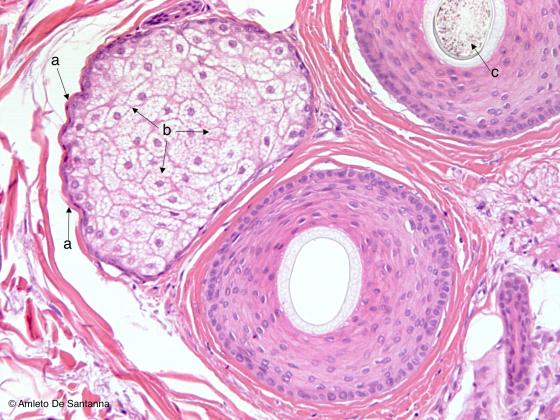
Figure E147. Human skin. Scalp micrograph at higher magnification. In the sebaceous gland, you can see two types of cells: slightly flattened or cuboidal cells at the border of the gland that are staminal cells (a), at the center of the gland there are larger, more roundish cells with a cytoplasm rich in lipid droplets. These are real secreting cells (b). Hair follicle (c). H&E X100
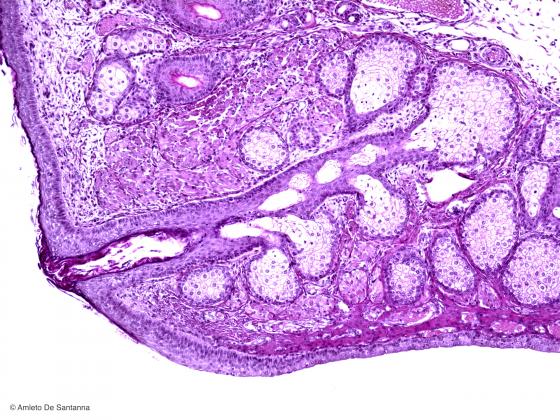
Figure E148. Human eyelid. Meibonium exocrine gland at small magnification. You can see the excretory duct that empties at the eyelid surface. H&E X20

Figure E149A. Human eyelid. Tarsal glands (Meibonium glands) (G). Tarsal glands are sebaceous exocrine glands that tend to group as a bunch around a single long duct (D). Mallory-Azan X63
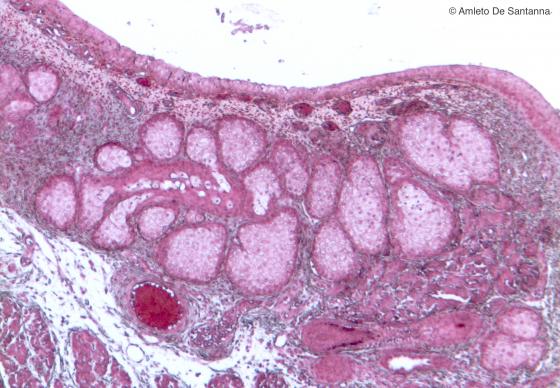
Figure E149B. Human eyelid. Tarsal glands (Meibonium glands). Mallory-Azan X63
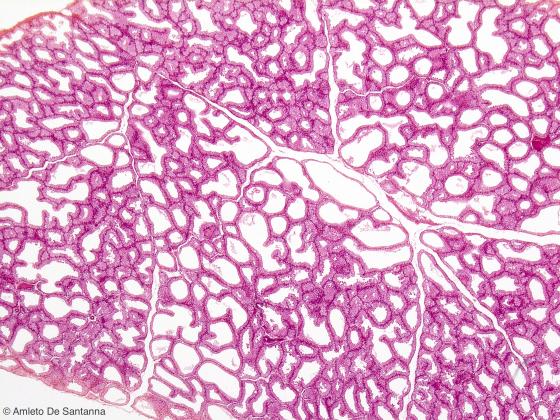
Figure E150. Human lacrimal gland. The lacrimal gland consists of lobules separated by connective septa composed of serous secreting tubuloacinar secretory units. H&E X40
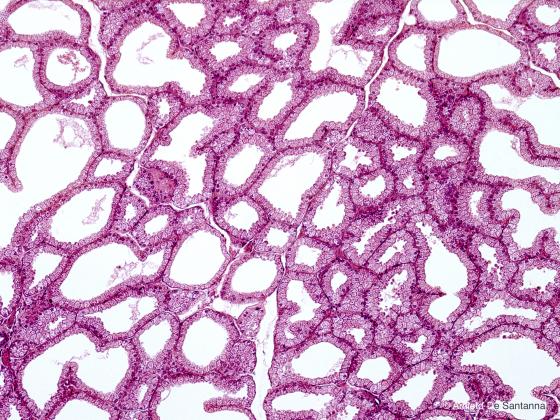
Figure E151. Human lacrimal gland at higher magnification. H&E X100
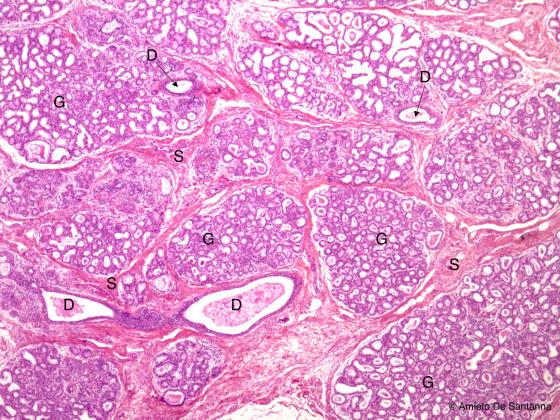
Figure E152A. Human mammary gland during lactation. Compound tubuloacinar gland. The micrograph shows the elongated or roundish secretory units with an evident duct (G). You can identify the lactiferous ducts (D) because of the dimensions and of the tall epithelium. The mammary gland is separated in lobules by connective septa (S) and the muscular component is very low. H&E X25
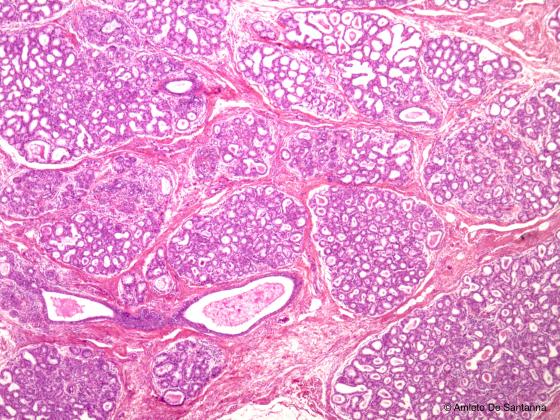
Figure E152B. Human mammary gland. H&E X25
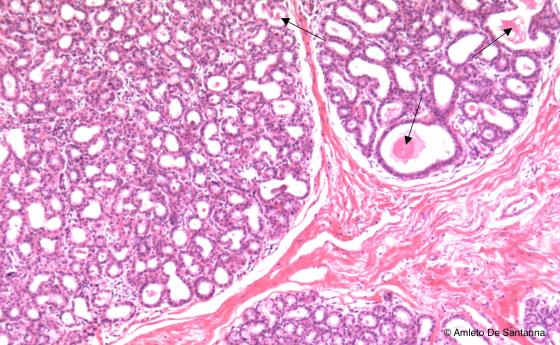
Figure E153. Human mammary gland during lactation. Compound tubuloacinar gland. You can see the secretion product (milk) in several duct (arrows). Differently from the prostate gland, in the mammary gland there are few muscle fibers and the alveoli are tightly packed. H&E X63
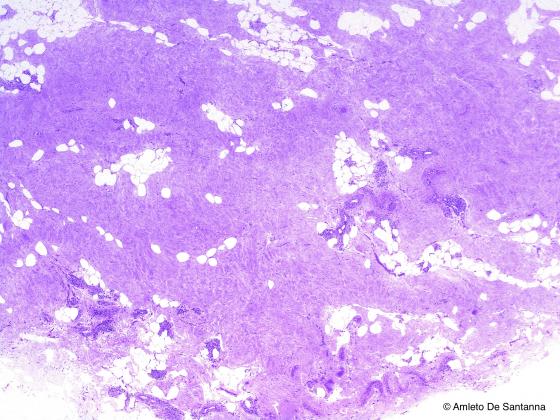
Figure E154. Human senile mammary gland. You can see the large amount of connective infiltrate and the degeneration of the glandular tissue. H&E X25
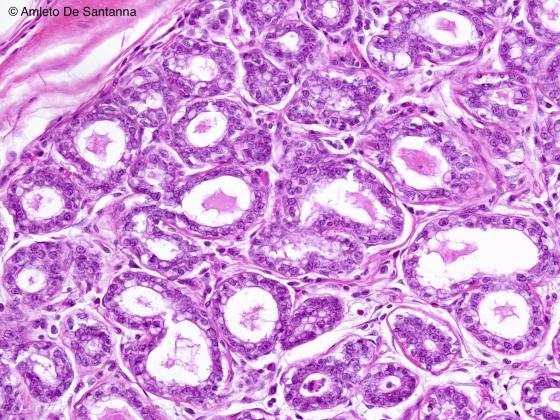
Figure E155. Human mammary gland during lactation at high magnification. H&E X200
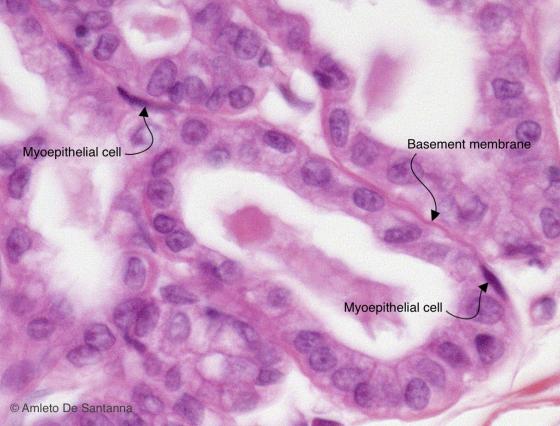
Figure E156. Human mammary gland during lactation at high magnification. Between the basement membrane and the lining epithelium of the secretory ducts you can see myoepithelial cells. These cells have a star-like shape and, inside the cytoplasm, they present actin and myosin fibers organized similarly to smooth muscle cells. Myoepithelial cells are present outside the acini and tubules of the gland propelling, with their contraction, the secretion product towards the opening of the gland. H&E X200
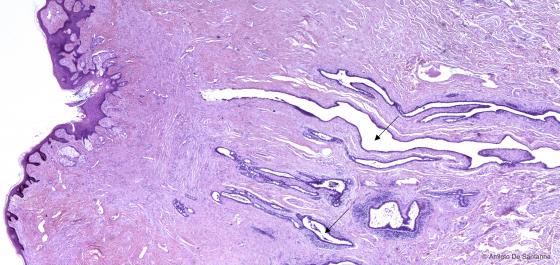
Figure E157. Human mammary gland. Lactiferous ducts in the nipple (arrows) H&E X20
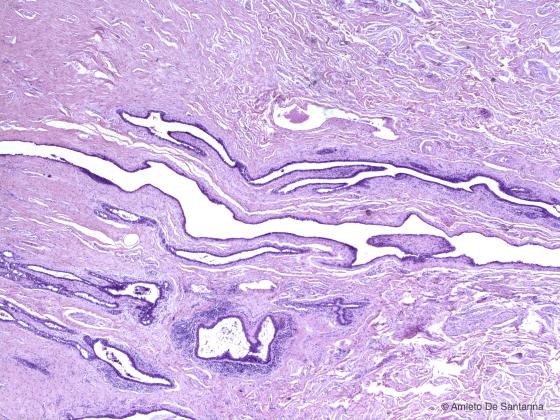
Figure E158. Human mammary gland. Lactiferous ducts at higher magnification. H&E X40
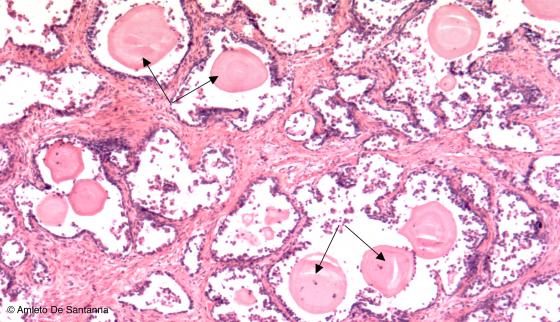
Figure E159. Human prostate gland. Compound tubuloacinar gland. You can see the distinctive features also at low magnification: elongated secretory units and evident lumina. Prostate gland differs from the other tubuloalveolar gland, the mammary gland, because of a strong muscular component that surrounds the secretory units and because of the presence of formations, variable in shape and number, called corpora amylacea (arrows). H&E X63
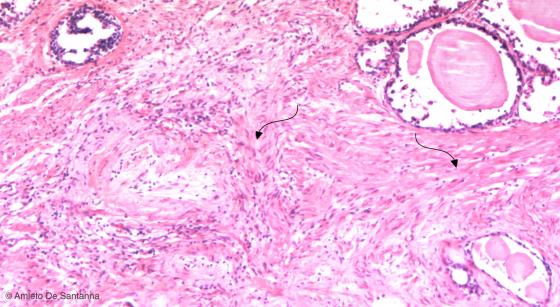
Figure E160. Human prostate gland. Low magnification micrograph that highlights the great amount of smooth muscle fibers surrounding the prostate secretion units (arrows). H&E X100
Endocrine glands
These glands produce a specific type of molecules, generally known as hormones, whose aim is to regulate the function of the specific organs they are produced for (known as target organs). Hormones can be either amino acid or lipid derived.
There are pure endocrine glands, composed exclusively of endocrine tissue, and amphicrine glands, composed of both endocrine and exocrine tissue (for example: the parenchyma of pancreas, generally marked by exocrine secretion, presents cell conglomerates with endocrine activity: the pancreatic islets – or islets of Langerhans).
Endocrine glands are classified in:
- Endocrine glands with solid epithelial cords: secretory cells form cell cords which are variably located in space. Most of endocrine glands belong to this type: hypophysis, parathyroids, adrenal glands, epiphysis, placenta, corpus luteum;
- Follicular endocrine gland: here the secretory part is represented by follicles lined by cells that produce a precursor of thyroid hormones (thyroglobulin), the only example of which is the thyroid gland;
- Islets endocrine glands: the pancreatic islets of Langerhans;
- Interstitital endocrine glands: these glands can be found in ovaries and in the interstitial space between the seminiferous tubules of testicles, in groups of six, eight or more cells surrounding a capillary in which they release the secretory substance (testosterone).
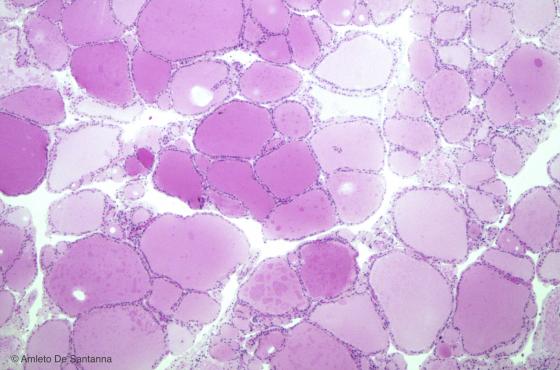
Figure E161. Human thyroid gland. The thyroid gland is composed of thyroid follicles, the functional units of the gland. These follicles are lined by a simple cuboidal epithelium (follicular cells or thyrocytes) and contain a gel-like substance called colloid. The thyroid gland is the only endocrine gland with this kind of structure. H&E X40
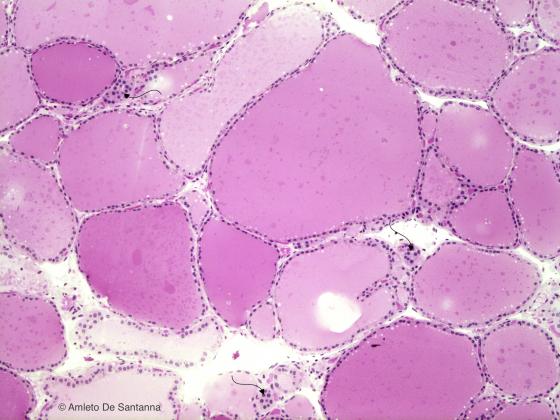
Figure E162. Human thyroid gland. The thyroid gland is compose of thyroid follicles, the functional units of the gland. These follicles are lined by a simple cuboidal epithelium (follicular cells or thyrocytes) and contain a gel-like substance called colloid. Near the follicles, you can see a few groups of parafollicular cells (arrows) H&E X63
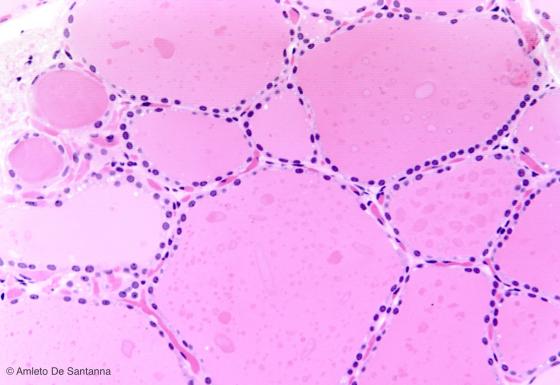
Figure E163. Human thyroid gland at higher magnification. H&E X100
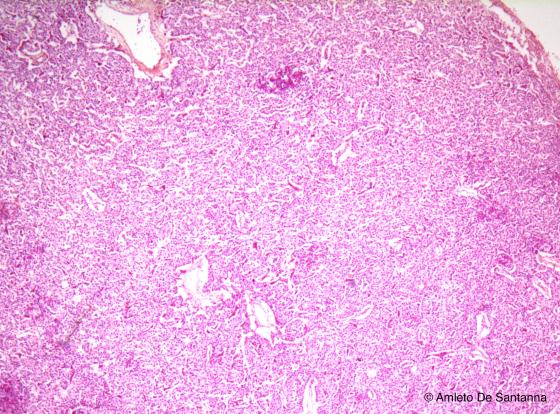
Figure E164. Human parathyroid gland. Endocrine gland with the parenchyma organized in cords of cells. H&E X40
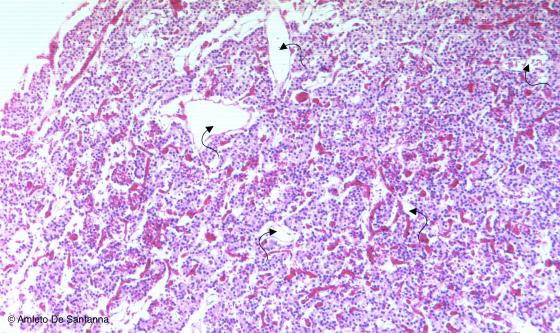
Figure E165. Human parathyroid gland. Endocrine gland with the parenchyma organized in cords of cells. You can identify the parathyroid glands on the base of the cords of endocrine cells and on the base of the presence of a large amount of blood capillaries (arrows) and of connective septa, stained red-orange. H&E X63
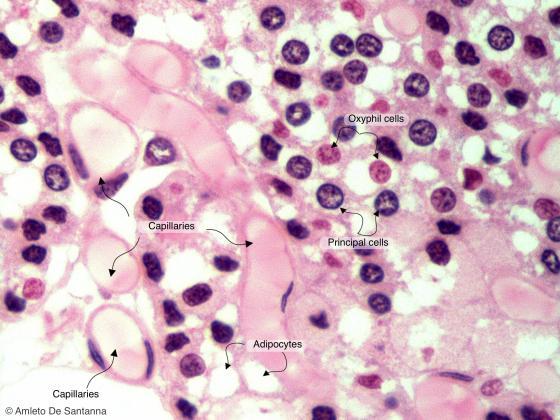
Figure E166A. Human parathyroid gland. Endocrine gland with the parenchyma organized in cords of cells. High magnification micrograph where you can identify the two cell types present in the parathyroid gland: principal or chief cells and oxyphil cells. H&E X1000
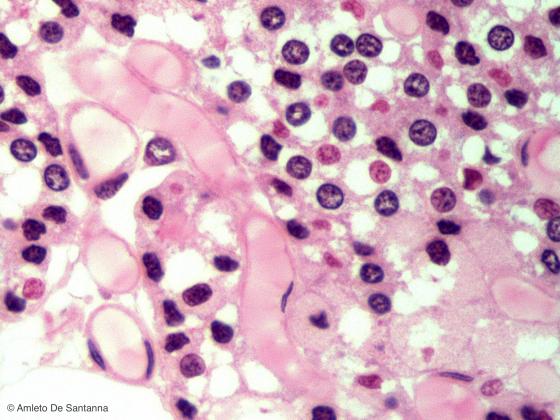
Figure E166B. Human parathyroid gland. Endocrine gland with the parenchyma organized in cords of cells. High magnification micrograph where you can identify the two cell types present in the parathyroid gland: principal or chief cells and oxyphil cells. H&E X1000
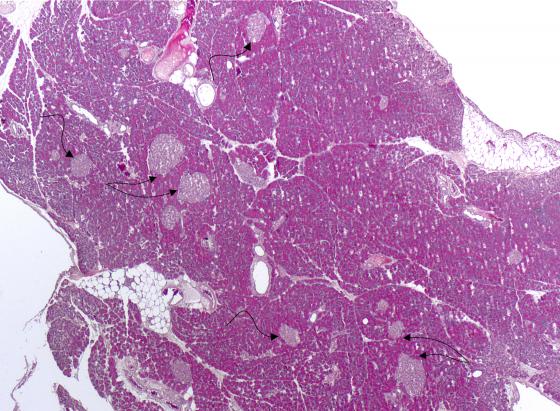
Figure E167. Rat pancreas. In this micrograph, you can see a large number of pancreatic islets (islets of Langerhans) (arrows). H&E X12.5
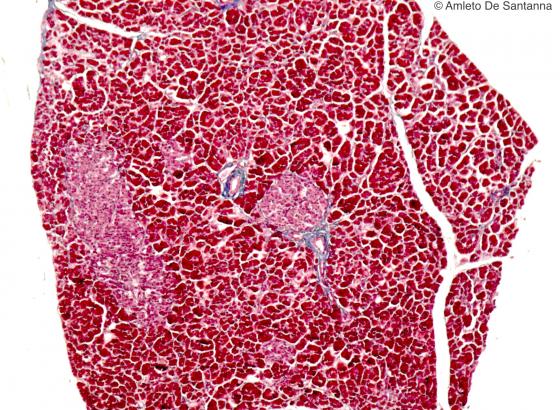
Figure E168. Human pancreas. The endocrine component of the pancreas in organized in cords of cells grouped to form an islet with endocrine secretion surrounded by exocrine tissue constituted of pancreatic acini. Azan X25
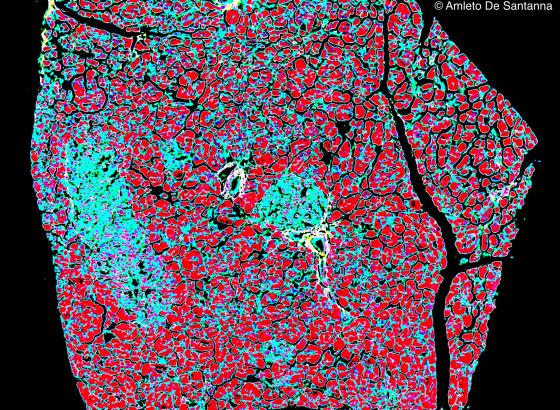
Figure E169. Human pancreas. The previous micrograph (E168) has been digitally processed to highlight blue the islets of Langerhans. X25
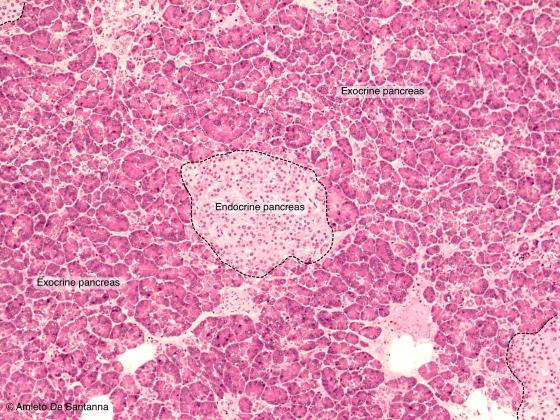
Figure E170A. Human pancreas. Micrograph at low magnification where you can see the different staining properties and the different organization of the exocrine and endocrine components of the pancreas. H&E X40
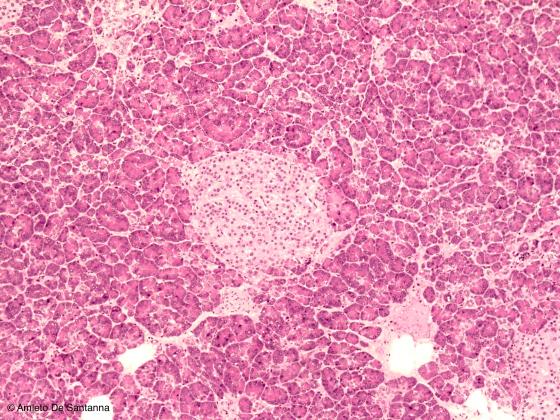
Figure E170B. Human pancreas. Micrograph at low magnification where you can see the different staining properties and the different organization of the exocrine and endocrine components of the pancreas. H&E X40
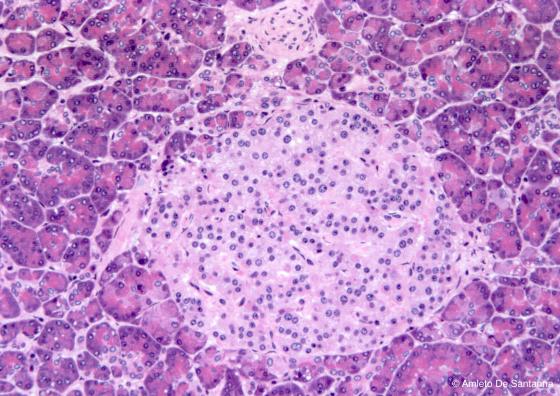
Figure E171. Human pancreas, islet of Langerhans. The endocrine component of the pancreas is organized in cords of cells grouped to form an islet with endocrine secretion activity, surrounded by exocrine tissue constituted of pancreatic acini. H&E X100
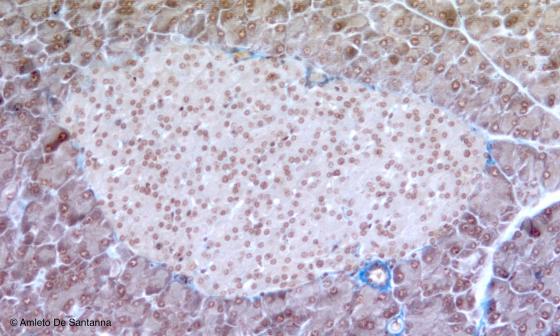
Figure E172. Mouse pancreas, islet of Langerhans. Ignesti X100
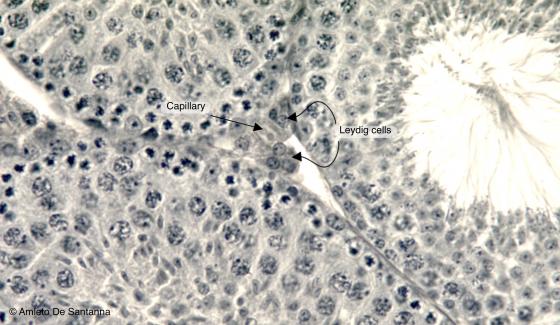
Figure E173. Mouse testis. Between the seminiferous tubules of the testis there are: connective tissue, blood vessels and endocrine cells called Leydig cells (or interstitial cells). Leydig cells secrete testosterone, responsible for the secondary sexual male characteristics. At the center of the micrograph, you can see an interstitial space with a blood capillary surrounded by a group of 5-6 large, globular, well stained cells: the Leydig cells. Iron hematoxylin X100
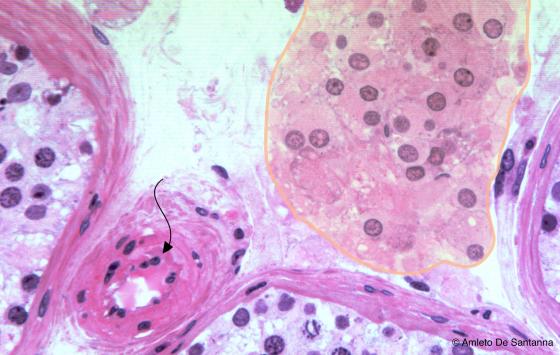
Figure E174A. Human testis. You can easily see Leydig cells (shadowed area) among seminiferous tubules and near a blood capillary (arrow), where the testosterone is secreted. H&E X200
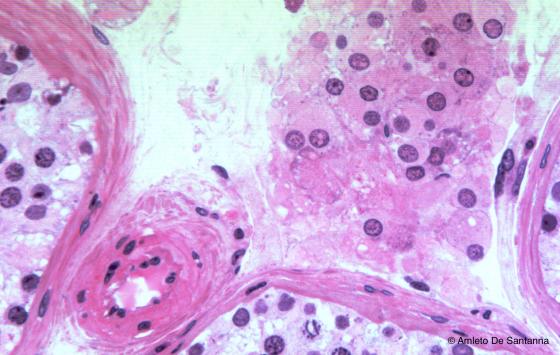
Figure E174B. Human testis. Leydig cells. H&E X200

Figure E175A. Rabbit adrenal gland. The adrenal gland has a connective tissue capsule, a cortex and a medulla. The adrenal cortex is divided into three zones: zona glomerulosa, zona fasciculata and zona reticularis. The inner medulla is easy to identify because is paler and rich in blood vessels. The adrenal gland is an endocrine gland that secretes two classes of hormones: steroid hormones (mineralcorticoids, glucocorticoids and adrenal androgens) in the cortex and catecholamines (epinephrine and norepinephrine) in the medulla. Mallory trichrome staining X40
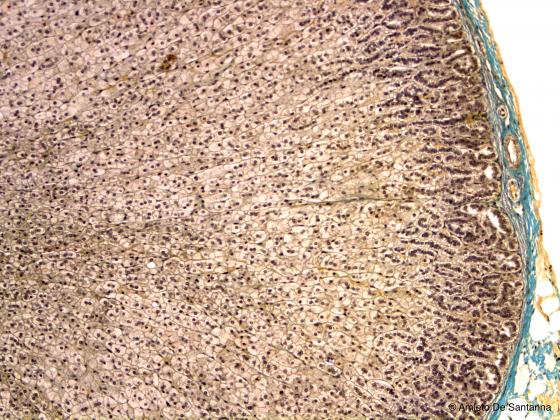
Figure E175B. Rabbit adrenal gland. Mallory trichrome staining X40
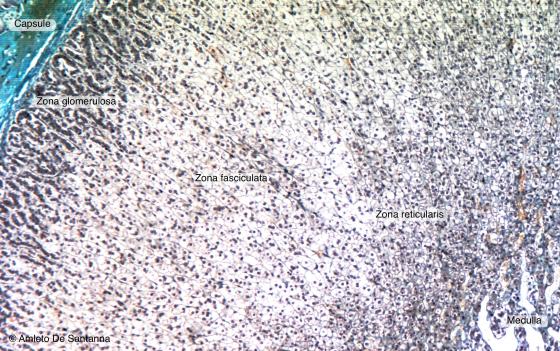
Figure E176. Rabbit adrenal gland. The adrenal gland has a connective tissue capsule, a cortex and a medulla. The adrenal cortex is divided into three zones: zona glomerulosa, zona fasciculata and zona reticularis. The inner medulla is easy to identify because is paler and rich in blood vessels. The adrenal gland is an endocrine gland that secretes two classes of hormones: steroid hormones (mineralcorticoids, glucocorticoids and adrenal androgens) in the cortex and catecholamines (epinephrine and norepinephrine) in the medulla. Mallory trichrome staining X63
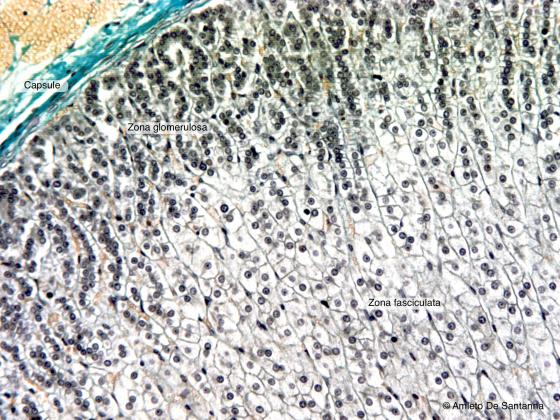
Figure E177. Rabbit adrenal gland. Endocrine gland with the parenchyma organized in cords of cells. Under the thick connective capsule, stained bright blue-green, the cords of cells have a short glomerular course that make them coil up: this is the zona glomerulosa. Subsequently, the cells spread piling up in parallel columns: this is the zona fasciculata, much larger than the zona glomerulosa. Mallory trichrome staining X100
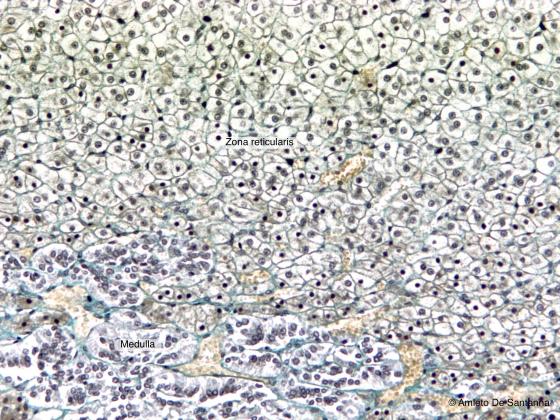
Figure E178. Rabbit adrenal gland. In this micrograph, you can easily see part of the zona reticularis and part of the medulla. In the zona reticularis, the cords of cells have a web-like organization. Mallory trichrome staining X100
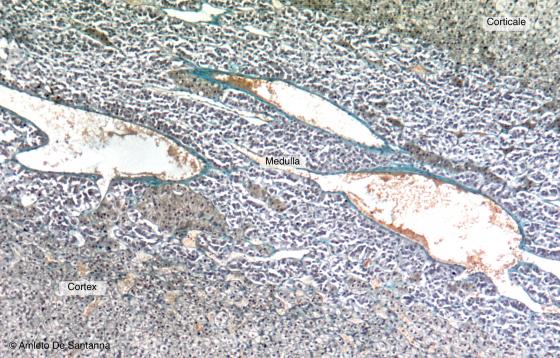
Figure E179. Rabbit adrenal gland. Adrenal medulla. The adrenal medulla is made up of a lower amount of cells than the cortex and there is a large number of blood vessels within a thick connective web. Mallory trichrome staining X63
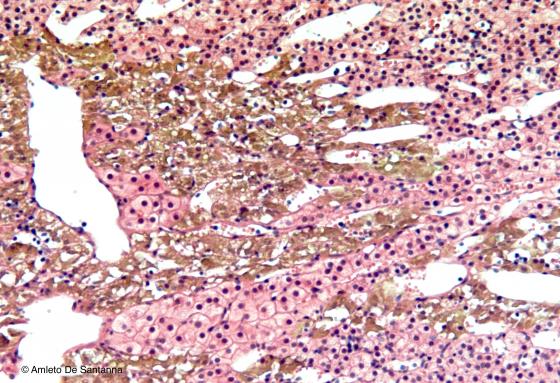
Figure E180. Human adrenal medulla. In addition, the parenchyma of the medulla is organized in cords of cells. With this histochemical staining, the chromaffin cells are highlighted brown. These cells are defined chromaffin because they have the ability to precipitate chromium salts due to the presence of catecholamines (epinephrine and norepinephrine). IHc X100
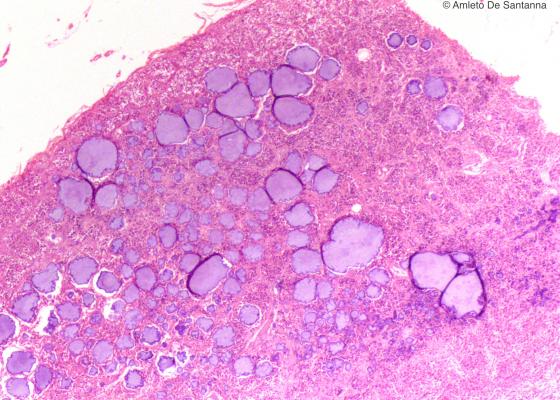
Figure E181. Human pineal gland. Endocrine gland with a parenchyma organized in cords of cells. H&E X25
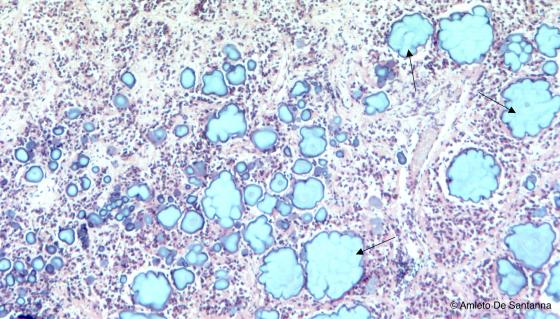
Figure E182. Human pineal gland. Endocrine gland with a parenchyma organized in cords of cells. You can see the cords of cells and, in the stroma, characteristic calcium salt formations that increase in number with age (arrows). H&E X63
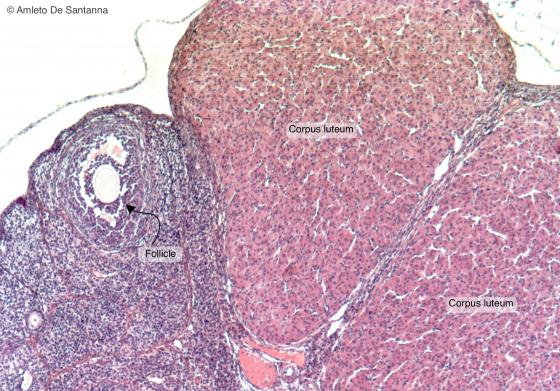
Figure E183. Mouse ovary. In this micrograph are present endocrine glands in solid epithelial cords: the corpora lutea. H&E X63
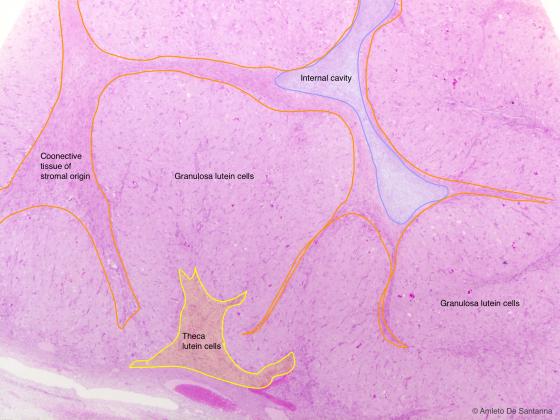
Figure E184A. Human corpus luteum during pregnancy. The corpus luteum is an endocrine gland organized in cords of cells. After ovulation, the ovarian follicle undergoes drastic changes. The follicle wall collapses forming deep folds and the cells of the stroma migrate inside the cavity. The granulosa cells, that are in a large number, bigger in size and less stained, become the granulosa lutein cells. The theca interna cells, smaller and more deeply stained, become theca lutein cells, and are positioned peripherally near the connective wall. Both cell types secrete hormones. H&E X100
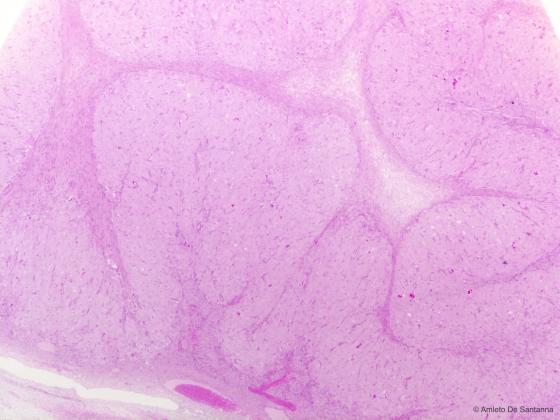
Figure E184B. Human corpus luteum during pregnancy. H&E X100
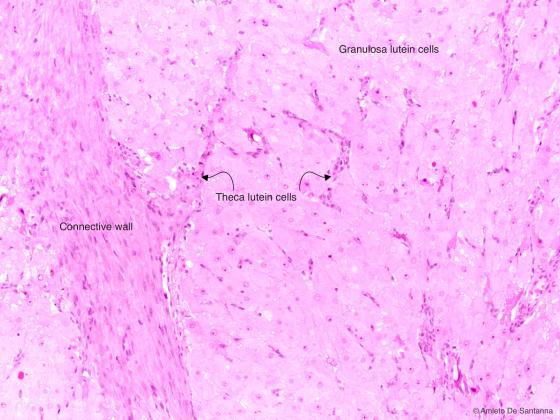
Figure E185. Human corpus luteum during pregnancy. The corpus luteum is an endocrine gland organized in cords of cells. In this micrograph, you can see the different morphology of the granulosa lutein cells, roundish with a central nucleus, compared to theca lutein cells, deeply stained with eosin and with an elongated nucleus. The connective wall of the corpus luteum is formed by cells deriving from the theca externa cells of the follicle. H&E X200
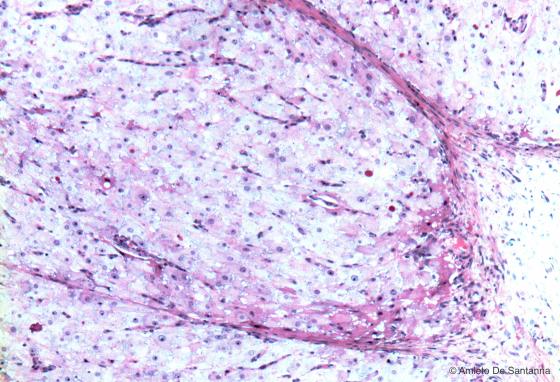
Figure E186. Human corpus luteum during pregnancy. The corpus luteum is an endocrine gland organized in cords of cells. The lutein cells, large, globular cells with a uniform shape, are organized in cords of cells. H&E X200
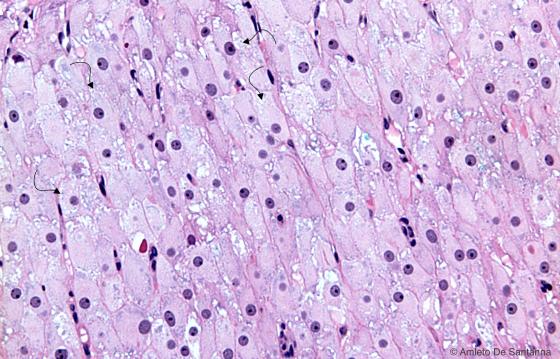
Figure E187. Human corpus luteum during pregnancy at higher magnification. You can see the organization in cords of the granulosa lutein cells, showing in the cytoplasm the characteristic lipid droplets (arrows). H&E X400
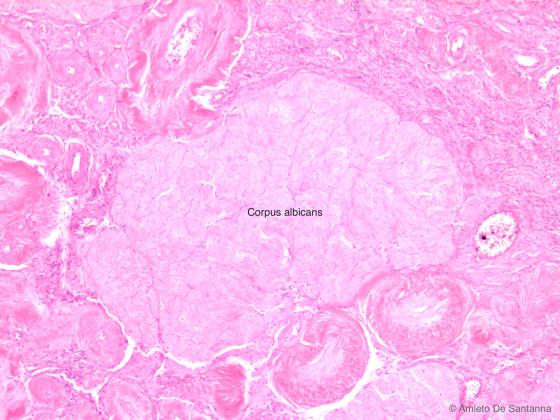
Figure E188. Human corpus albicans. If the oocyte is not fertilized the corpus luteum degenerates into a corpus albicans, identifiable as a poorly stained mass. H&E X100
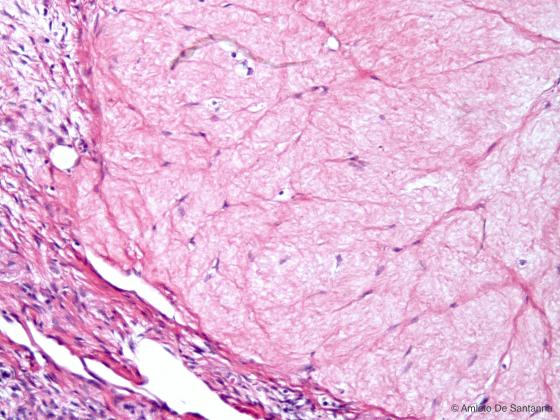
Figure E189. Human corpus albicans at higher magnification. H&E X200
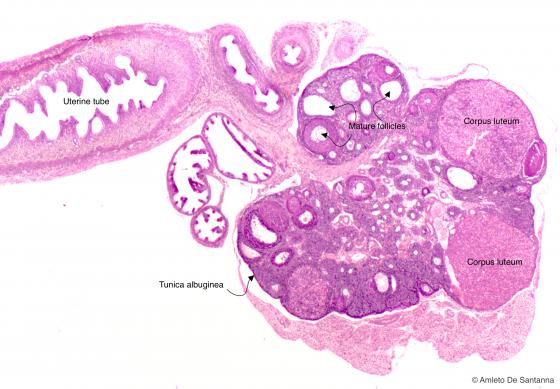
Figure E190. Mouse ovary at low magnification. H&E X25
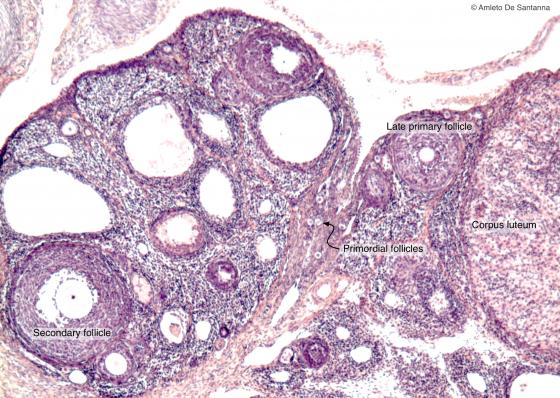
Figure E191. Mouse ovary. Overall view of a mouse ovary where you can see follicles at different maturation stages and a corpus luteum. H&E X100
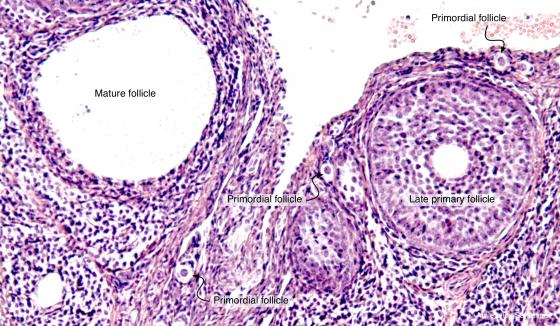
Figure E192. Mouse ovary. You can see follicles at different maturation stages. H&E X100

Figure E193A. Human ovary. Follicle at maturation where you can see the different elements. H&E X100

Figure E193B. Human ovary. Follicle at maturation. H&E X100
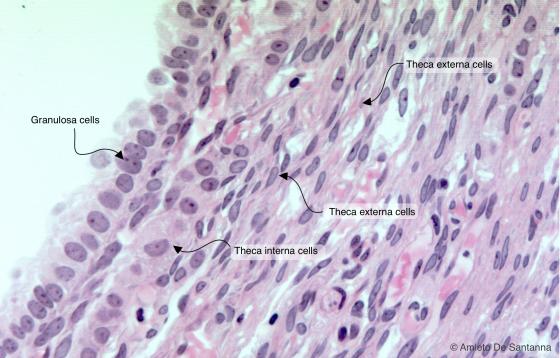
Figure E194. Human ovary at high magnification. You can easily identify the theca interna endocrine glands placed between the granulosa cells and the theca externa cells. H&E X200
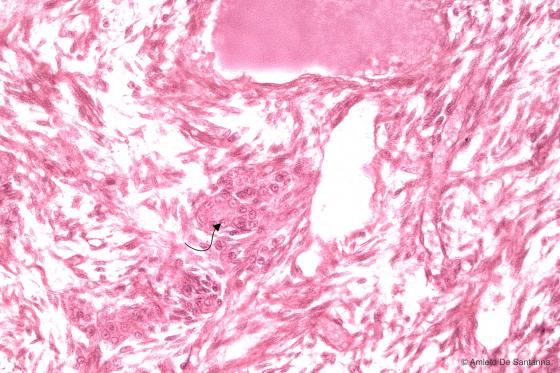
Figure E195. Human ovary. Leydig cells of the ovary (arrows). The Leydig cells of the ovary are organized in cords and secrete testosterone. H&E X250
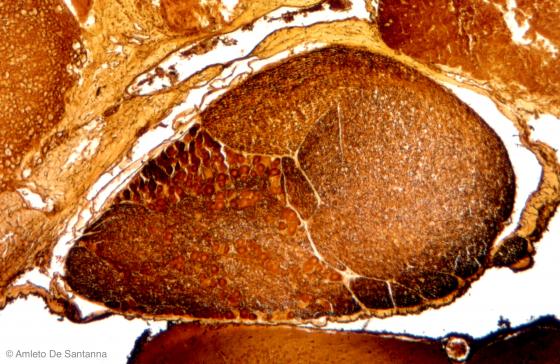
Figure E196. Human fetal pituitary gland. The pituitary gland is an endocrine gland that secretes several hormones. In this micrograph you can see it located into the sella turcica (turkish saddle), a depression of the sphenoid bone at the base of the skull. Golgi-Cox X63
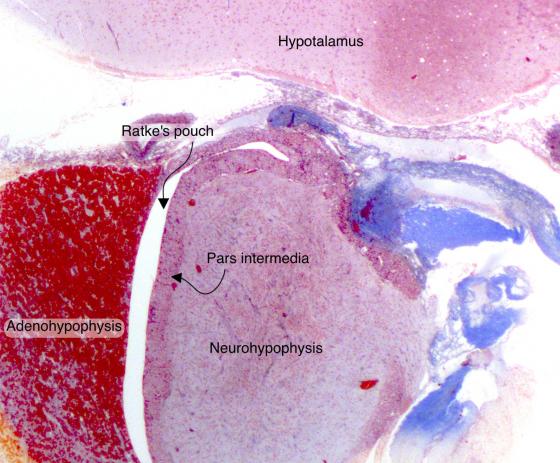
Figure E197. Human pituitary gland. The pituitary gland is an endocrine gland composed of three parts: the adenohypophysis (anterior lobe), the pars intermedia and the neurohypophysis (posterior lobe). The adenohypophysis and the pars intermedia are made of cords of cells. Masson trichrome staining X25
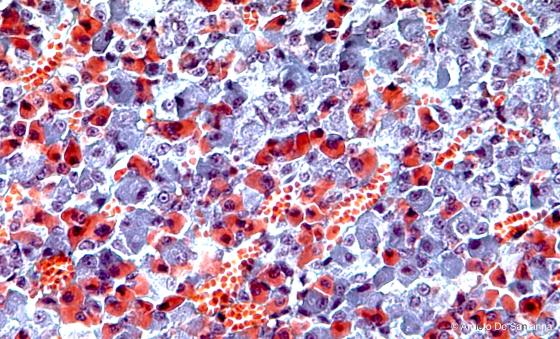
Figure E198. Anterior lobe (adenohypophysis) of a human pituitary gland. In the anterior lobe, you can identify different cell types: chromophilic cells, deeply stained, and the chromophobic cells, poorly stained. Chromophilic cells are divided into acidophils, with a basic cytoplasm and stained orange-red, and basophils, with an acid cytoplasm and stained purple. Masson trichrome staining X200